Non-Surgical Spinal Decompression Centre
Melbourne Australia

Spondylolisthesis
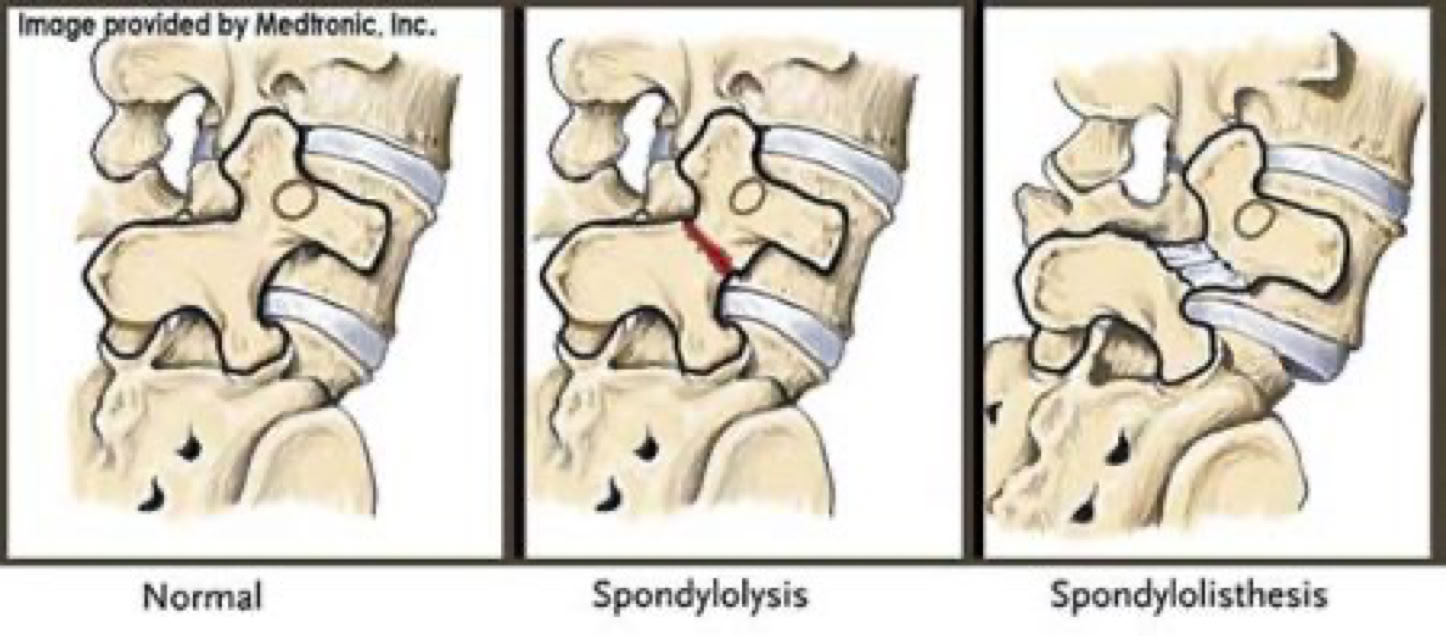
Spondylolisthesis refers to the forward displacement of one lumbar vertebra relative to the vertebra beneath it. This condition can arise from various mechanisms, with the two primary causes being stress fractures in the vertebra and degenerative changes in the facet joints.
Anatomy
To fully understand how these mechanisms lead to slippage, it’s important to first grasp the anatomy of the vertebral motion segment. Each level of the spine functions as a three-joint complex: two facet joints at the back and a large intervertebral disc in the front. This "tripod" structure provides significant stability, supports the weight above each spinal level, and facilitates movement in all directions. When the disc remains healthy, it can effectively absorb these forces over many years without causing symptoms.

Spondylolysis:
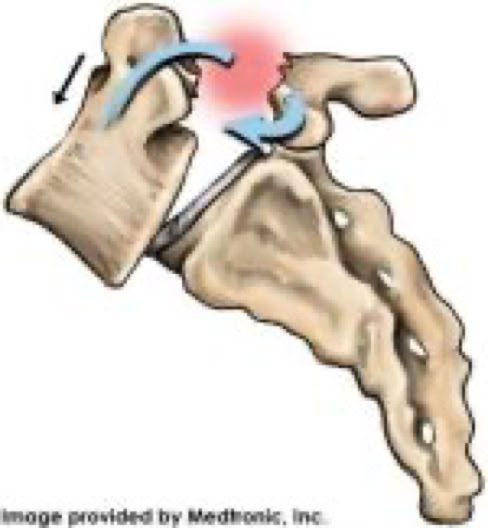
Spondylolysis, also known as a pars fracture or stress fracture, occurs when there is a break in a delicate part of the vertebral bone called the "pars." This fracture typically affects both sides of the pars and can lead to spondylolisthesis, where a vertebral body slips forward. In simpler terms, a stress fracture in this area may cause the vertebra to shift out of place.
The fracture can result from several factors, including direct trauma, repetitive strain—particularly from high-impact sports—or inherent weaknesses in the bone due to genetics. The pars is a small, thin bone that, when repeatedly stressed (similar to bending a paperclip back and forth until it breaks), can fracture. This condition is most commonly seen in adolescents, with estimates suggesting that 5-7% of teens may be affected. It's particularly prevalent in athletes engaged in sports involving heavy impact or rotational forces.
The good news is that most pars fractures heal with rest and a strengthening program targeting the core muscles. In cases where the bone doesn’t heal fully, the body may form fibrous scar tissue to provide some support.
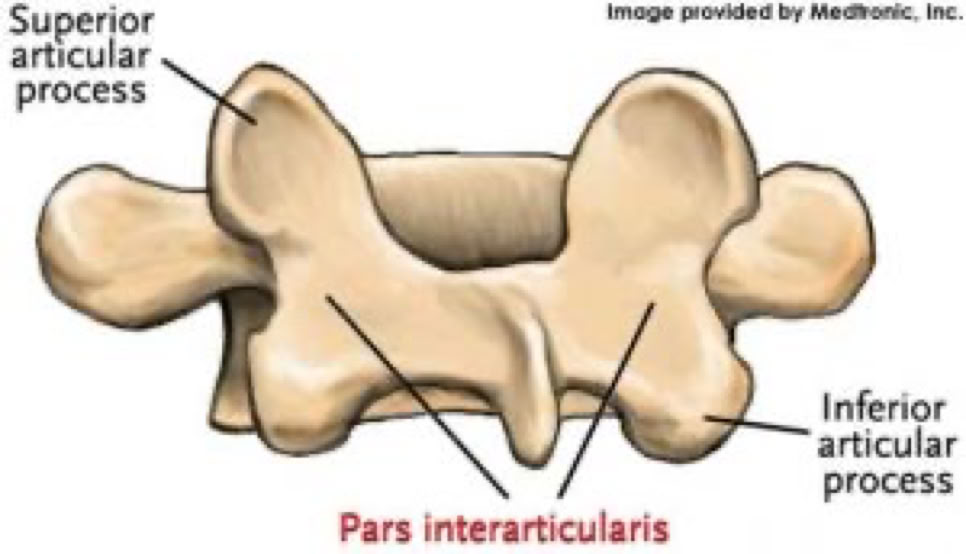

A VIEW FROM THE BACK OF A VERTEBRA SHOWING THE PARS.
The pars acts as a bony hook, and when it fractures, it compromises the posterior support of the vertebra. Over time, this can lead to forward slippage of the vertebra. Many individuals with spondylolysis experience no symptoms for years, as their discs remain healthy. However, a stress fracture reduces the posterior support of the vertebral segment, placing additional strain on the disc in front. This increased stress can contribute to degenerative disc disease, where the disc gradually deteriorates and fails to adequately support the bone above. As the disc degenerates, the collagen fibers break down, causing the disc to lose water. When the disc dehydrates, it loses both height and function, and its narrowing can result in abnormal movement between the bones above and below. Moreover, the fracture gap at the pars can widen, leading to further forward shifting of the vertebra—known as spondylolisthesis. This process can be compared to a tripod stool with two back legs partially cut through: over time, the stool becomes unstable and tips forward. Similarly, any abnormal movement between vertebrae signifies segmental spinal instability, as these bones are not supposed to move in such a way.
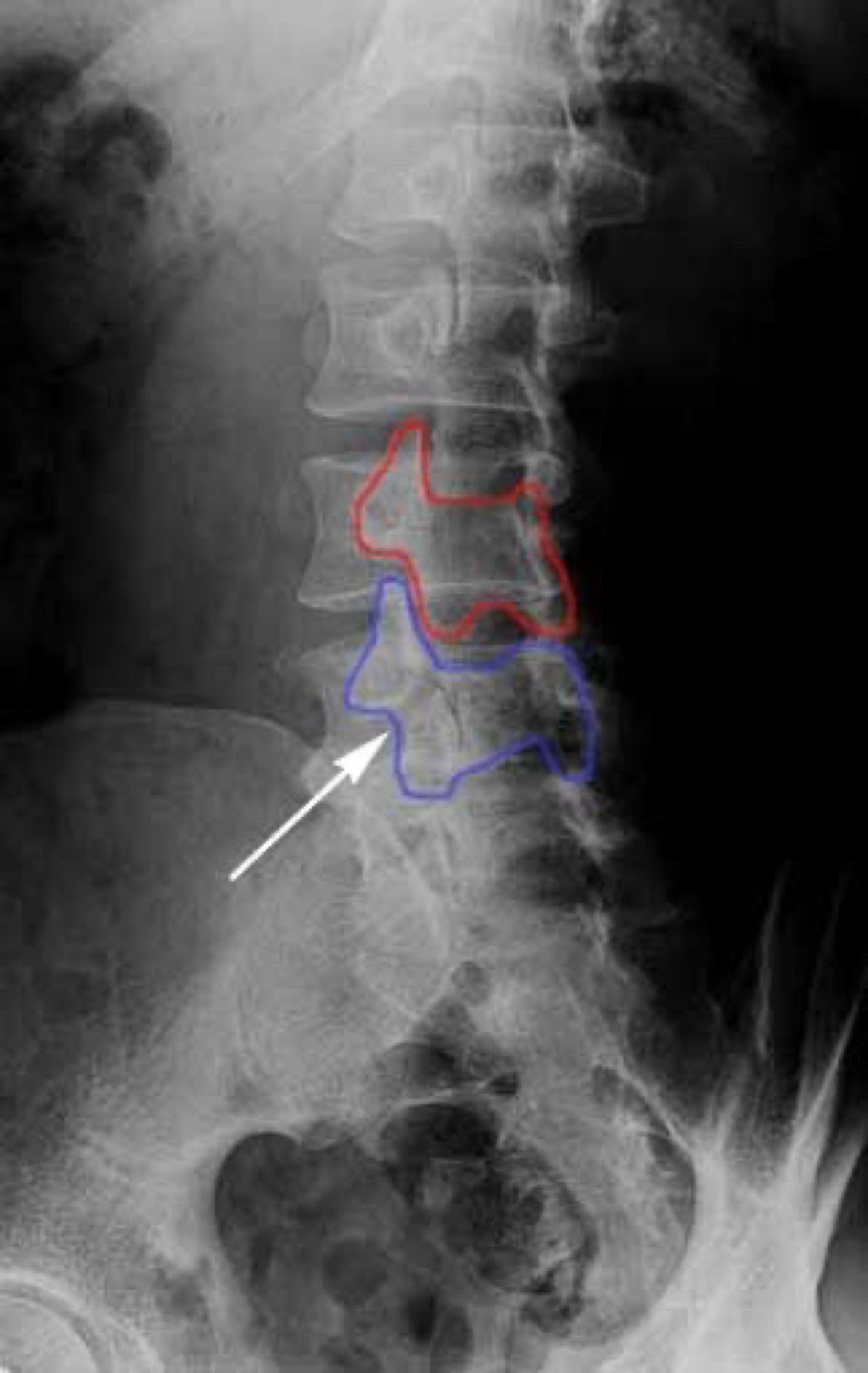
When we look at the spine from the side, we can imagine a scotty dog. It is outlined above. The pars fracture is seen as a collar around the dog's neck. Instability and movement can cause the neck to widen. We will see this below in an X-ray example.
Facet Joints and Spondylolisthesis:
One of the primary causes of spondylolisthesis is the acquired degeneration of the facet joints. These joints are located at the back of the spine, forming part of the three-joint complex that provides stability and support. To understand this better, a review of spinal anatomy might be helpful.
As the facet joints undergo degeneration, the small ligaments that help stabilize them weaken and loosen. These ligaments play a crucial role in maintaining joint integrity, much like the ACL in the knee. When these ligaments lose their firmness, the facet joints become more mobile and can separate abnormally during movement. This increased separation can contribute to pain, as well as allow the intervertebral disc to shift forward, exacerbating the condition.
Diagnosis:
Spondylolisthesis is most commonly observed in the lumbar spine, which bears the majority of the body’s weight. To evaluate spinal instability, X-rays are typically taken while the patient bends forward (flexion) and backward (extension). Under normal conditions, there should be no significant motion at the affected level. However, increased movement between the flexion and extension X-rays often correlates with more pronounced symptoms, indicating a greater degree of instability and discomfort for the patient.


X-RAY SHOWING A PARS FRACTURE DEFECT
THE WHITE OUTLINE SHOWS THE SLIPPAGE.
Most symptoms can be effectively managed without surgery. The deep core muscles of the abdomen play a crucial role in supporting and stabilising the lower back. Strengthening the core is a key component of treatment. Depending on a patient's level of core strength, the spine may experience different degrees of instability.
Treatment
If there is no instability in the lumbar spine, Non-Surgical Spinal Decompression can effectively create an opening and promote a pumping action to alleviate symptoms.
However, if there is instability in the lumbar spine, surgical intervention may become necessary, especially if symptoms progress to severe back pain, leg pain, or significant neurological issues caused by a pinched nerve. The primary goal of surgery is to stabilise the affected spinal segment. This is most commonly achieved through spinal fusion, a procedure that permanently joins the slipping vertebrae to prevent further movement and reduce pain, but unfortunately, it can create hypermobility in the segments above or below the fusion over time.
© 2025 Dr. Ilan Sommer DC (USA), Phone# 1300662295 Send us an Email